Understanding Diverticulosis and Diverticulitis
What is Diverticulosis
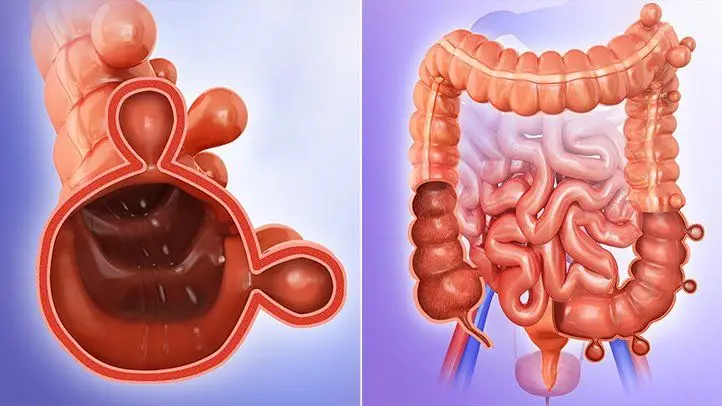
Diverticulosis is the presence of pockets or pouches that push through the wall of the bowel, and fortunately they don’t cause any problems most of the time. Diverticulosis can lead to diverticulitis, as you will see below.
Symptoms of Diverticulosis
For the majority of people, they are not even aware that they have diverticulosis, as they experience no symptoms. For some people, though, they will experience symptoms, the most common being bloating, constipation, abdominal pain. It is important to remember that having these symptoms does not mean you have diverticulosis, as other bowel conditions can present in similar ways. It is in fact possible to have these symptoms, but not have any structural damage to your intestinal wall, as is the case with irritable bowel syndrome (IBS).
Management of Diverticulosis
If you have no symptoms, a high fibre diet and anti-inflammatory foods, with a focus on having a range vegetables and fruit, whole grain products, nuts, seeds, legumes and fish. This not only supports the beneficial bacteria in your gut, but also has other health benefits too, including heart health.
If you have symptoms then dietary management involves 2 aspects:
- Step 1 is determining whether there are some foods that are causing symptoms due to the digestive process. Some foods, for example certain fruits and vegetables, wheat products, alternative sugars, are fermented in the gut. These foods can contribute to changes in bowel motions and abdominal pain and bloating. It is essential that any food elimination is done appropriately, as many of these foods are beneficial to gut health. In addition, if it is done appropriately, it reduces the length of time you need to eliminate foods to get answers – generally my clients will have an answer within 3 weeks.
- Step 2 is to promote those foods that actually improve the integrity of the gut and encourage health gut bacteria. Gut bacteria play a key role in your immune system, they aid digestion, and also play a role with brain health.

What is Diverticulitis
Diverticulitis occurs when the pouches in the colon (i.e. the diverticula) become infected or inflamed. There are different classifications for diverticulitis. Skip through this if you are not interested in the detail.
- Acute and uncomplicated. With this inflammation of the bowel wall has occurred, but no abscess or perforation, in other words a hole through the bowel wall, has occurred.
- Acute and complicated. In this instance, perforation (in other words breaking through of the wall of the colon) has occurred and may result in an abscess i.e. swelling of tissue with pus. In severe cases, it can result in actual faeces in the abdominal area.
- Chronic and uncomplicated. With this the inflammation continues and the walls of the abdominal area thicken.
- Chronic and complicated. This results in the opening in the colon narrowing (stenosis) and can result in a blockage.
Symptoms of Diverticulitis
- Pain, which may be constant and persist for several days. The lower left side of the abdomen is the usually where the pain is experienced.
- Nausea and vomiting.
- Fever.
- Abdominal tenderness.
- Constipation or, less commonly, diarrhoea.
Management of Diverticulitis
Management is aimed at reducing inflammation and infections.
During the initial occurrence of diverticulitis, dietary management may include a low fibre diet. After this, the focus is as for diverticulosis – it is aimed at identifying foods that aggravate symptoms, and then to support gut health and minimise ongoing symptoms.
Usually medical management is a part of this in the form of antibiotics to manage the infection. Recent research has suggested that medications aimed at reducing the inflammatory process, may be more beneficial in the management of chronic diverticulitis.
Who is most likely to get Diverticulosis or Diverticulitis?
You are at increased risk of diverticular disease (diverticulosis or diverticulitis) if you:
- Are over 40 years of age.
- Are male.
- Are genetically predisposed. This accounts for up to 50% of susceptibility(i.e. makes you most likely) of getting it.
- You don’t eat a lot of fruits, vegetables, beans and legumes, breads and grains or nuts and have a diet high in processed foods.
- Don’t exercise.
- Take non-steroidal anti-inflammatory medicines, like Brufen; steroids or opiates on a regular basis. This has been shown to increase the risk by 70%
Where can I get help?
Your GP is always the best starting point. He may refer you onto a specialist. For dietary help, a registered dietitian with experience in gut health can help you identify potential food triggers and then ensure that you are following the optimum diet to protect your gut and manage your symptoms. If you would like to book an appointment or discuss this further, click this link
- Vanhauwaert, E., Matthys C., Verdonck, L. and De Preter, V., 2015. Low-Residue and Low-Fiber Diets in Gastrointestinal Disease Management. Advances in Nutrition, 6 (6), pp. 820-827.
- Latella, G., Pimpo, M., Scottili, S., Zippi, M., Viscido, A., Chiaramonte, M. and Frieri, G., 2003. Rifaximin improves symptoms of acquired uncomplicated diverticular disease of the colon. International Journal of Colorectal Disease, 18 (1), pp 55-62.
- Bianchi, M., Festa, V., Moretti, A., Ciabo, A., Mangone, M., Tornatore, V., Dezi, A., Luchetti, R., De Pascalis, B., Papi, C. and Loch, M., 2011. Meta-analysis: long-term therapy with rifaximin in the management of uncomplicated diverticular disease. Alimentary Pharmacology and Therapeutics, 33 (8), pp 902-910.
- Schultz, J.m Azhar, N., Binda, G., Barbara, G., Biondo, S., Boermeester, M., Chabok, A., Consten, E., Dijk, S., Johanssen. A., Kruis, W., Lambrichts., Post, S., Ris, F., Rockall. T,. Samuelsson, A., Di Saverio, S., Tartaglia, D., Thorisson, A., Winter, d., Bemelman, W. and Angenete, e., 2020. European Society of Coloproctology: guidelines for the management of diverticular disease of the colon. Colorectal Disease, 22 (S2), pp. 5 -28.